Anatomy and Physiology: Where It All Happens
Where It All Happens
Are you a coffee addict? I have to get up very early because the first class I teach is at 7:30 A.M. My biggest complaint is when coffee tastes too weak; brown water doth not a good cup of coffee make! I remember asking someone behind the counter at some coffee house if the coffee was strong. His answer showed no understanding of the science behind coffee, which, surprisingly enough, has an awful lot to do with nephrons!
The young man behind the counter said that the beans were strong, and that was the only thing that mattered. While it's true that some beans have a stronger flavor than others, simple logic tells you that strong coffee has to have more dissolved solutes. The simplest way is to make the coffee with more coffee beans! In the same way, stronger, darker urine, which is produced when the body has to preserve water, has less water and thus more solutes.
Another way to make the coffee stronger, in other words to get more solutes into the water, is to grind the beans smaller. The smaller the grind, the greater the surface area to volume ratio of the beans, and the greater the ratio, the more solutes get into the coffee. In the same way, the proliferation of capillaries in the development of the kidney—in particular the cluster of about 50 fenestrated (see Cardiovascular and Lymphatic Circulation) capillaries in the glomeruli (singular, glomerulus), where the solutes first leave the capillaries—leads to a greater SA/V in the kidney. The higher the SA/V ratio in the kidneys, the stronger the urine you'll make!
If you are a real coffee aficionado, then you have probably discovered espresso, that rich, strong coffee. So what's the secret to making espresso so strong? It's more than just a finer grind (although espresso grind is extremely fine). The secret is the use of steam rather than hot water. What's the difference? The steam is at higher pressure, which increases the strength of the filtration process.
In the nephron (see Figure 15.3), the blood enters the glomerulus through an afferent (entering) arteriole, flows through the fenestrated capillaries of the glomerulus, and then exits through a smaller efferent (exiting) arteriole. Just like putting your thumb over the end of a flowing garden hose, the smaller size of the efferent arteriole increases the pressure. The higher the pressure, the stronger the filtrate (the material that is filtered out), or, in this case, the urine. That means that we have two little espresso makers in our body! Just don't start drinking your urine!
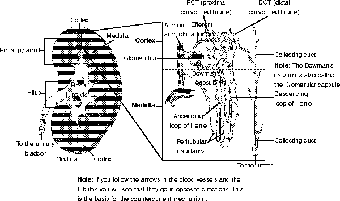
Figure 15.3The structure of a nephron, the part of the kidney where the urine is actually made. (LifeART©1989-2001, Lippincott Williams & Wilkins)
Smooth muscle cells that wrap around the afferent arteriole and the distal convoluted tubule (which we will meet shortly) are used to help regulate blood sugar. This odd ring of muscle has a rather scary name, hidden behind an innocuous abbreviation: the JGA, or juxtaglomerular apparatus (the thing near the glomerulus, or words to that effect). Blood pressure is also regulated through a hormone called renin, which is released by the cells of the JGA.
Renin converts a plasma protein from the liver called angiotensinogen into angiotensin I, which in turn is turned into angiotensin II in the lungs. Angiotensin II raises blood pressure, especially in the glomerulus (the start of the nephron); it also stimulates the release of aldosterone from the adrenal glands (see Hormones) and the subsequent reabsorption of Na+ ions (which helps to reabsorb the water—see the countercurrent mechanism). Stimulating thirst also helps raise blood volume, as does angiotensin II's habit of stimulating the release of ADH, or antidiuretic hormone, which prevents water loss in the urine. All in all, that's a pretty busy schedule of hormonal activities!
The Big Picture
This connection between the kidneys and blood pressure in the cardiovascular system has ramifications for blood pressure medication. Higher blood pressure, as indicated in the discussion of renin and angiotensin II, leads to less urination. In order to lower blood pressure, one type of medication, called a diuretic, relaxes the JGA and causes a release of more water in the urine. This is why diuretics make you pee!
Next, I'd like you to look at the structure of the nephron. There are two basic parts, the renal corpuscle, where the fluid is filtered (made of the Bowman's capsule and the glomerulus), and the renal tubule, actually a series of tubules, where the filtered fluid travels. These tubules are, in order, the proximal convoluted tubule or PCT (named both for its proximity to the glomerular capsule and for its twisted shape), the loop of Henle (with its descending limb and its ascending limbs), the distal convoluted tubule or DCT, and finally the collecting duct (which we mentioned earlier, the start of the collecting system). Each portion of the renal capsule, as we shall see, differs in its structure, as well as its function in the urine-making process.
Filtration
Filtration is the process of selectively removing, or filtering, materials out of a solution, and it happens in the glomerulus, producing a protein-free fluid, filtrate, that is somewhat akin to blood plasma (see Figure 15.4). The only problem is that blood has an awful lot of things we don't want put in the urine, not to mention things we do want to release! Now that it is in the filtrate, we have to get the good stuff back, and the job of getting it back will be discussed in the next section.

Figure 15.4Filtration in the glomerulus. (©Michael J. Vieira Lazaroff)
I already mentioned the afferent and efferent arterioles, on the other end of the glomerulus, and the high pressure produced that helps with the filtration, but what about the rest of the renal corpuscle? The glomerulus lies in a capsule known as the glomerular capsule or the Bowman's capsule. This capsule is made of simple squamous epithelium, which makes up the parietal epithelium. The visceral epithelium consists of cells called podocytes, which have numerous small “feet” called pedicels. These pedicels, and the basement membrane (called the lamina densa), help to keep the proteins from entering the filtrate.
An amazing amount of filtrate is produced every minute. The glomerular filtration rate (GFR) is about 125 ml a minute, or about 10 percent of the volume of the blood entering the kidney. One of the reasons this is possible is the enormous filtration surface of 6 m2 per kidney. Once the filtrate leaves the capillaries, the coils and loops of the renal tubule, and the capillaries around them, called peritubular capillaries, change the concentration of the filtrate, through reabsorption and secretion.

Excerpted from The Complete Idiot's Guide to Anatomy and Physiology © 2004 by Michael J. Vieira Lazaroff. All rights reserved including the right of reproduction in whole or in part in any form. Used by arrangement with Alpha Books, a member of Penguin Group (USA) Inc.
To order this book direct from the publisher, visit the Penguin USA website or call 1-800-253-6476. You can also purchase this book at Amazon.com and Barnes & Noble.







